DIABETES AND THE EYE
About Diabetic Retinopathy
Diabetes can affect the eye in a number of ways. Uncontrolled or poorly controlled diabetes can lead to swelling of the lens inside the eye causing the power of the spectacles to fluctuate or vary. Diabetics may develop recurrent lids infections like styes Diabetics tend to develop cataract earlier and the cataract “matures” faster.
Diabetes can affect the eye in a number of ways.
li>Uncontrolled or poorly controlled diabetes can lead to swelling of the lens inside the eye causing the power of the spectacles to fluctuate or vary.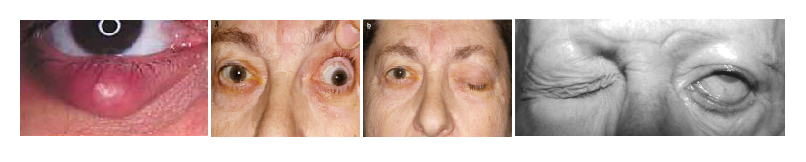
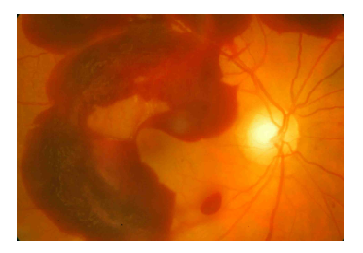
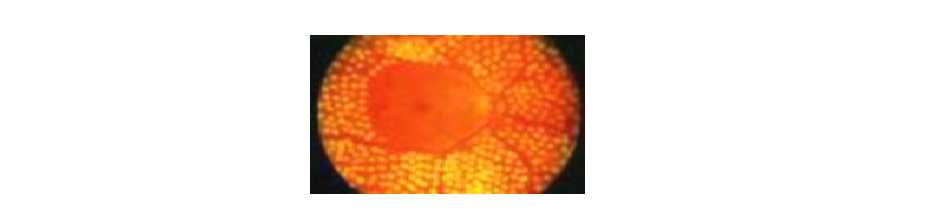
The retina is a light sensitive film lining the internal surface of the back of the eye. The most sensitive part of the retina is called the macula and it is with this we read and watch TV, etc. To be able to work properly, the retina needs a good blood supply. A single blood vessel entering the back of the eye divides into many smaller branches-each of which supplies its own portion of the retina. Damage to these blood vessels leads to diabetic retinopathy. Though Retinopathy usually develops after the patient has been diabetic for a while (7-10 years on an average), sometimes it is on finding retinopathy that the diabetes is detected.Mild diet controlled diabetics can still have a severe retinopathy.
Once the blood vessels of the retina are affected, it can cause a number of problems
Well-controlled diabetes delays the onset of diabetic retinopathy, but does not always prevent it.
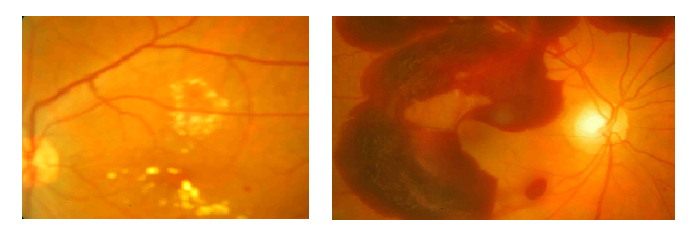
The different types of maculopathy are determined by :
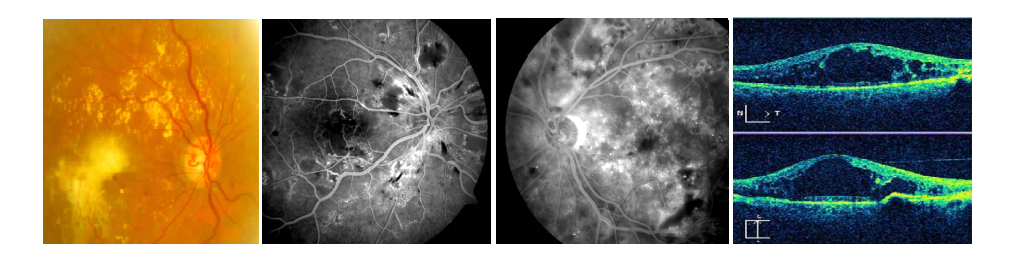


Presence of associated anemia, kidney disease, raised blood pressure and dyslipidemia(abnormal cholesterol etc levels) increases the risk of worsening of diabetic retinopathy and blood tests may be advised to determine if these are present



