GLAUCOMA
About Glaucoma
Diabetes can affect the eye in a number of ways. Uncontrolled or poorly controlled diabetes can lead to swelling of the lens inside the eye causing the power of the spectacles to fluctuate or vary. Diabetics may develop recurrent lids infections like styes Diabetics tend to develop cataract earlier and the cataract “matures” faster.

The commonly occurring types of glaucoma are PRIMARY GLAUCOMA-occur without any known cause.
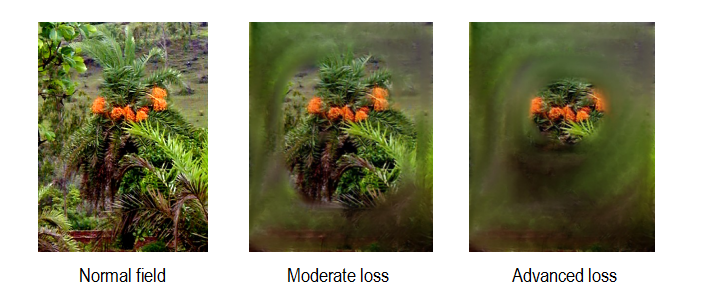
Primary glaucoma, usually affects both eyes though one is often more severely affected than the other. During the early stages the pressure within the eyes slowly damages the nerve. The optic nerve, in healthy eyes has about one million nerve fibers. In glaucoma, over a variable period of time (months to years), the nerve fibers die because of the high pressure or lack of adequate blood supply within the eye. The higher the eye pressure the faster the damage occurs Routine tests can detect damage only after about 20-40% damage has occurred. Initially the side vision and dim light vision is affected, central vision remaining normal. When 90% of the fibers have been damaged the patient begins to notice blurring of central vision. Between when the damage first becomes detectable and when the patient first notices a problem the damage can be detected by careful examination of the optic nerve at the back of the eye and by field tests (perimetry) which assess the side vision.
Most often there are no symptoms until very late in the disease process. Symptoms like
These are not specific of glaucoma, but may be the first signal. One variant of glaucoma- the angle closure glaucoma can occasionally(but not always) produce symptoms like severe headache with pain in the eye and blurred vision with colored haloes around lights, early in the disease process before much damage has occurred. Patients of congenital glaucoma(present at birth or in early childhood) usually have large/prominent eyes with watering and excessive sensitivity to light.
The diagnosis of glaucoma is made based on the
The aim of all treatment is to prevent further damage to the eye and side vision from glaucoma. We cannot reverse the damage that has already occurred, but with modern treatment it is possible to slow or prevent further damage from occurring, provided the patient strictly follows the doctor’s instructions. Not all patients with pressures over 20 need treatment-while some with pressures of 16 or 17 may need treatment. If you are suspected to have glaucoma you will be reassessed to confirm the diagnosis. In the clinic, we sometimes want to measure the eye pressures a number of times before deciding the type of treatment.
Please do use your drops every day as instructed even if you are coming for a check up. Do try and be regular about coming for your check up as advised by the doctor. Timing of the drops is of importance-please try to follow the schedule advised by the doctor.
Treatment does not guarantee protection from further worsening-so repeated follow up and monitoring is essential, changes being made to the treatment as necessary
Once your eye pressure and optic nerve condition is stable, you will be asked to come back for follow up at 4 monthly intervals. Long term stability will require less frequent follow ups. Even though your eye pressure is controlled and you are using your eye drops regularly, there may be spikes in eye pressure between clinic visits which may go unnoticed. Hence, you will be required to undergo perimetry and or OCT tests at regular intervals to confirm that the damage is not getting worse.
Your vision may be affected by other problems in the eye like cataract, macular degeneration, diabetic changes in the retina, blocked blood vessels etc, which can co-exist. Surgery for cataract can now be combined with glaucoma surgery if required, with excellent results.


